Milk does the body good whether you’re 10 or 50, and for a similar reason: bone health. The big difference is that at 10 years old you’re building bone strength, at 50, you’re trying to preserve it.
Osteoporosis is a condition that causes bones to become brittle and fragile, and it’s more common in women than men. Bone fractures attributed to osteoporosis affect an estimated 1.5 million people annually. They can seriously impact one’s health and quality of life.
Bone density and osteoporosis
Doctors can screen for osteoporosis by testing your bone density or how strong your bones are. Bone density, or bone mineral density (BMD), is the amount of bone mineral in bone tissue. Testing BMD is the only way to know for sure that you have osteoporosis. At Welia Health, we use a dual energy X-ray absorptiometry or DEXA, which is the most common test for osteoporosis. Doctors measure bone density at the hip and spine, as these areas provide a good idea of whether you’re likely to fracture other bones in your body.
Screening recommendations
There has been some controversy over osteoporosis screening, largely surrounding a perception that pharmaceutical companies were pushing to lower recommended screenings to increase demand for osteoporosis drugs to drive profits. Medical associations such as the American Academy of Family (AAFP) Physicians and the American College of Obstetrics and Gynecology (ACOG) and have similar guidelines, which we follow at Welia Health.
American Academy of Family Physicians
- Recommends against DEXA screening in women younger than 65 years and men younger than 70 years with no risk factors
American College of Obstetrics and Gynecology
(2012/Reaffirmed 2014)
- Recommends BMD testing with DEXA beginning at age 65 years in all women
- Recommends selective screening in postmenopausal women younger than 65 years who have osteoporosis risk factors or an adult fracture
Risk factors for osteoporosis
Around age 50, both women and men experience increased bone loss. Women tend to lose more bone as they transition into menopause, given the loss of estrogen. The hormone plays an important role in replacing older bone with newer dense bone, throughout a woman’s life. (In men, testosterone converts to estrogen to build bone mass.)
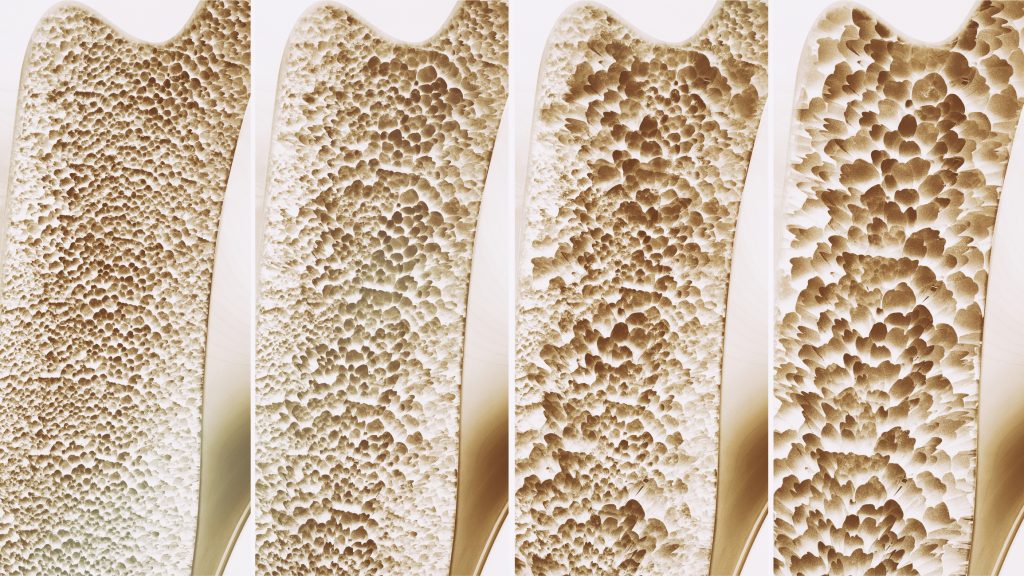
From left to right: healthy bone, osteopenia, osteoporosis, severe osteoporosis.
Although bone loss starts to occur around 50, the medical guidelines don’t call for screening until age 65, unless there are risk factors beyond sex, age and race (you’re at greatest risk if you’re white or of Asian descent). Your Welia Health provider can help you determine whether you have risk factors that merit a screening before 65 years old. Some of the risk factors include:
Family history. Having a parent or sibling with osteoporosis puts you at greater risk, especially if your mother or father fractured a hip.
Body frame size. Women (and men) with small body frames are at higher risk because they might have less bone mass to draw on as they grow older.
Thyroid problems. Too much thyroid hormone can cause bone loss, which can occur with an overactive thyroid or taking too much thyroid hormone medication to treat an underactive thyroid. Osteoporosis has also been associated with overactive parathyroid and adrenal glands.
Dietary factors. Osteoporosis is more likely to occur in people who have had low calcium intake throughout their lives, as the latter contributes to lower BMD. Eating disorders or severely restricting food intake can also weaken bones. Gastrointestinal surgery can also increase osteoporosis risk because when you reduce the size of your stomach or remove part of the intestine, it limits the amount of surface area available to absorb nutrients, such as calcium.
Steroids and other medications. Long-term use of oral or injected corticosteroid medications (e.g. prednisone and cortisone) disrupts the bone-rebuilding process. Other medications connected to osteoporosis risk include medications used to treat:
- Seizures
- Gastric reflux
- Cancer
- Transplant rejection
Medical conditions. Osteoporosis can also be more common in people who have:
- Celiac disease
- Inflammatory bowel disease
- Kidney or liver disease
- Cancer
- Lupus
- Multiple myeloma
- Rheumatoid arthritis
- Alcoholism
Lifestyle choices. Many of the risk factors above are out of your control. But some are not. The lifestyle choices that affect your osteoporosis risk include:
- Inactivity: People who are sedentary have a higher risk of osteoporosis. Any weight-bearing exercise and activities that promote balance and good posture are helpful for your bones. But walking, running, jumping, dancing and weightlifting seem particularly helpful.
- Excessive alcohol consumption: Regularly drinking more than two alcoholic drinks a day increases your risk of osteoporosis.
- Tobacco use: Tobacco contributes to weak bones, though its exact role in osteoporosis isn’t clear.
If you’re concerned about osteoporosis, talk to your Welia Health provider and learn what you can do today to lower your risk or to determine if a screening is right for you.












